In the process of childbirth, I experienced a third-degree tear extending from my vagina to my anus, leading to a combined pelvic organ prolapse. Facing challenging physical and psychological difficulties, I encountered shame, misjudgment, and ignorance. For months, doctors dismissed my pain as emotional until I was finally properly diagnosed and began my long journey to recovery. In my experience within the German health system, there’s a strong push for vaginal birth, labeled as ‘natural,’ with reassurances that complications are minimal. Yet, my vagina was broken. Wasn’t my injury foreseeable? And is there a happy ending to my story?
The question is: Why do broken vaginas happen? Every maternal birth injury is different and requires specific medical attention, yet women worldwide often suffer silently. While we can’t foresee every complication during childbirth, expectant mothers should not be deprived of the comprehensive data necessary for making informed decisions about their birth, its risks, and postpartum care. The study results and statistics of maternal birth injuries I researched were shocking.
This article documents my journey through the agony and confusion of untreated birth complications, gaps in education for perinatal healthcare providers, and my long search for answers. I delve into the reality of maternal birth injuries in Europe, explore their sources, and try to understand the reasons behind the widespread problem affecting millions of women worldwide. And finally I discuss various treatments, including pelvic floor physiotherapy, neural therapy, reconstructive surgery, and aesthetic gynecology, offering hope and information to women facing similar struggles.
It is time to break the silence and provide much-needed support and solidarity.
My Unexpected Journey Through Childbirth
In September 2020, I undertook on the journey of childbirth, anticipating the joy of welcoming my baby girl. However, what followed was a traumatic experience that shattered my expectations and left me with profound physical and emotional distress. Despite my careful physical and mental preparation during pregnancy, my labor stretched agonizingly over 26 hours, culminating in the loss of 1.5 liters of blood and a third-degree tear extending from my vagina to my anus. The violence of childbirth were mixed with the overwhelming love and pride I felt upon seeing my daughter for the first time.
After the birth, I remained unaware of the extent of my injuries. Reassured by the doctor who stitched me after delivery and subsequent medical examinations, I returned home to take care of my newborn. However, the months that followed were marked by persistent physical pain and emotional anguish. My lower pelvic area ached with discomfort, accompanied by sensations of heaviness and dragging, a foreign body feeling, urinary and fecal incontinence, and a profound sense of unease. My vagina protruded outward to such an extent that I found myself pausing frequently to manually push the prolapsed tissue back inside with my fingers, just to maintain some sense of normalcy in my daily life. It’s difficult to express how deeply this affected me; it felt like living a nightmare.
Even the intimacy of sexual intercourse became extremely painful, profoundly affecting the connection with my husband. I don’t think I need to elaborate on the toll it took on our relationship. The relentless cycle of pain, sleep deprivation, and exhaustion plunged me into a postpartum depression. I tried hard to be the best mommy and wife, masking my pain behind a busy day schedule, but I know my mental health affected them as well. I felt guilty about everything. Out of shame and fear of being misunderstood, I pushed my friends away and closed myself off, pretending I was fine. However, my suffering continued, making my situation even worse.
Honestly, I was literally wetting myself and leaking poop with every cough or laugh. I was afraid to go out. In my mind, I pretended this wasn’t happening to me. I learned to contract my pelvic floor muscles for hours just to make it through the day without any embarrassing incidents. I don’t think I was ever really honest with anyone about what was happening, not even with myself.
When I fully realized my new reality, I became extremely angry and sad at my fate, only to be judged by others: “You look angry! Aren’t you happy and grateful that you have a healthy baby?” a neighbor, a mother of two, once said to me. “God damn it, of course I am grateful, but I am furious as well! My vagina is hanging out, I cannot hold my pee, and everything hurts!” I thought to myself but said nothing and felt guilty for my lack of positivity. How dare I stigmatize the role of a mother and undermine her sanctity? One thing is certain, I never connected my birth injury with my baby girl. I love her; I do not blame her or myself for my injuries—how could I? She is my everything.
Before I continue, I want to make it clear that my intention is not to dissuade women from vaginal birth or to induce fear. My goal is to encourage deeper exploration of this subject and empower women to make informed decisions based on their unique circumstances. Every woman’s journey is different, and it’s essential to approach childbirth with thorough consideration and understanding. Postpartum injuries affect many women, and if you are one of them, this article can help you understand what happened, where to seek help, and what questions to ask on the road to recovery.
Please note that I am not a medical practitioner. My recommendations are based on my own experiences and research. Consult your prenatal care specialist, gynecologist, and/or physiotherapist for any medical questions.
Breaking the Silence
Feeling ashamed, I doubted the medical professionals who assured me that time would heal my issues. Despite their sugar-coated assurances, I couldn’t shake the feeling that my condition was far worse than they acknowledged. The conversations with my midwife, gynecologist, and hospital obstetricians seemed to gloss over the truth, leaving me unable to openly discuss my birth experience and subsequent condition. I struggled with feelings of disconnection from my own body and emotions.
During my distress, I feared I was losing my sanity. It seemed that crucial information had been deliberately withheld from me, as I later learned from my midwife: “For your own sake, to spare you unnecessary worry before the birth.” Such remarks echoed throughout my journey, dismissing my concerns with phrases like “It can’t be that bad”, “You must be overly sensitive”, “You probably have a lowered pain threshold”, “At least your baby is healthy”, “Your pain is ’emotional'”, “The way you feel is normal, it will pass.” Even more disheartening was the fact that many of these comments came from female doctors.
After seven months of desperate searching, I stumbled upon the German Pelvic Floor Center at Alexianer St. Hedwig Hospital in Berlin. Tears streamed down my cheeks as I entered the hospital, haunted by the fear of being dismissed once again. What if my ailment truly existed only in my mind? As I settled into the gynecology chair, I awaited yet another verdict. Moments later, the diagnosis pierced through the tension: Cystocele grade II, rectocele grade III, damage to the external sphincter, postpartum trauma to the perineal muscles. While the gravity of the diagnosis sank in, there was an unexpected sense of relief—I wasn’t imagining it after all.
“Why had nobody seen this before?” I fumed with anger. I felt deceived and manipulated, left to navigate my struggle alone. But now, armed with proper documentation of my condition and a recommendation for surgery post-breastfeeding, I was finally equipped with a plan. In the meantime, I was recommended temporary solutions: pelvic floor physiotherapy and the Vaginal Pessary, which I’ll discuss it later.
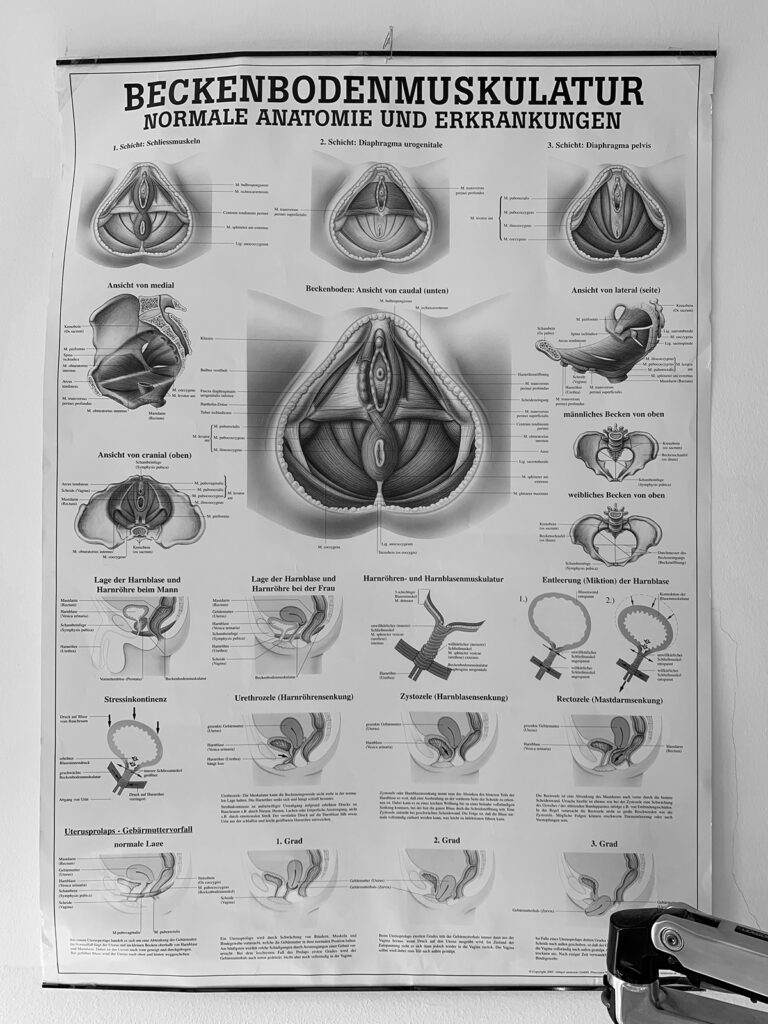
Why Do Broken Vaginas Happen?
I have asked myself this question many times before. One of the most enlightening reads that finally opened my eyes to the extent of the problem I was experiencing, was a book by Dr. med. Martina Lenzen-Schulte, Open at the Bottom – The Pelvic Floor After Childbirth: Belittled – Ignored – Tabooed (trans. from German). Dr. Lenzen-Schulte explains: “Why, many sufferers ask themselves, did we never hear anything about pelvic floor damage before giving birth? And why are we not taken seriously now? The two are connected. Many gynecologists and midwives do not know enough about pelvic floor damage. In the past, this was not part of the curriculum, it is still not a top topic in gynecology and not one in midwifery training.” 1 It’s no wonder that pregnant women and young mothers don’t understand the risks of postpartum injuries, as doctors and midwives are not properly trained in this area. Similar issues arise with perineal sutures used to repair tears or episiotomies during vaginal birth, often causing long-term discomfort and dyspareunia (painful intercourse) when done incorrectly. Dr. Lenzen-Schulte points out, “Everyone sews as they can. And everyone teaches how they sew” 1 (trans. from German). Inexperienced practitioners are often sent to birthing centers without proper supervision, highlighting the need for improved techniques and skills among midwives and obstetricians to ensure proper recovery.
In another eye-opening article, “Millions of Women Are Injured During Childbirth. Why Aren’t Doctors Diagnosing Them?”, Laura Beil brings forth the plight of women who suffered from postpartum depression and/or birth injuries. These women “have faced not only severe pain, but also misdiagnoses, delays in correct diagnosis, improper and unproven treatments, gender bias, stigma, and ‘neglect, dismissal and discrimination’ from the health care system.” 2 The author rightfully emphasizes the need for changes in education for healthcare professionals and expresses her disapproval of discounting women’s pain as “emotional.”
Addressing the multifaceted problem of birth injuries is complicated by underreporting due to shame, lack of awareness, inadequate education among medical practitioners, and the normalization of symptoms like urinary incontinence or perineal discomfort. Improved awareness, education, communication, and compassion among healthcare providers and patients are crucial. Postpartum assessments and follow-up care are essential for properly recognizing and treating maternal birth injuries.
I was surprised to learn how widespread birth injuries are. The UK foundation MASIC helps women who have suffered severe childbirth injuries by raising public awareness, supporting research, and educating medical professionals. Their statistics and real-life stories are very eye-opening. Here is one of those stories:
The Numbers Behind Maternal Birth Injuries
According to The American Journal of Obstetrics & Gynecology, “Perineal trauma after vaginal birth is common, with approximately 9 of 10 women being affected. Second-degree perineal tears are twice as likely to occur in primiparous births, with an incidence of 40%”. 3 Furthermore, the likelihood of developing pelvic organ prolapse (POP) due to vaginal birth, causing a bulging bladder, bowel, or uterus into the vagina, is also more common than expected. According to the National Health Services (NHS), “Research indicates that about 50% of women who have given birth may have a prolapse”. 4, 5 Slight perineal tears during natural births are unproblematic for most women. However, the incidence of pelvic organ prolapse, which varies widely and depends on many factors, is alarmingly high and should not be overlooked.
I’m not saying vaginal childbirth is always traumatic. Numerous women have healthy deliveries, but childbirth injuries still affect millions worldwide. “Many women experience labor-related and childbirth-related morbidity in the medium-to-long term after childbirth (i.e., beyond 6 weeks postnatally). Available data show the most prevalent conditions are dyspareunia (35%), low back pain (32%), urinary incontinence (8–31%), anxiety (9–24%), anal incontinence (19%), depression (11–17%), tokophobia (6–15%), perineal pain (11%), and secondary infertility (11%)”. 6 The numbers speak for themselves. Downplaying the incredible challenge a woman’s body goes through during pregnancy and childbirth is, in my opinion, unacceptable. Researchers from the University of Michigan found that childbirth is comparable to running a marathon. Their study of 68 women, conducted seven weeks postpartum, revealed that 29 percent had undetected fractures in their pubic bones, and 41 percent had undiagnosed tears in their pelvic floor muscles. 2
I’m also not suggesting that a caesarean section eliminates all the risk of birth injuries. “Giving birth by cesarean could prevent some birth injuries, but it is major surgery and carries risk. Carrying a pregnancy, regardless of how you give birth, puts strain on your pelvic floor and can cause pelvic floor injury”. 7 Therefore, understanding our bodies and learning about prevention methods are essential. We need to be able to make informed decisions based on our unique circumstances and medical records. Speak to your doctor, seek answers, and always trust your instincts.
Types of Birth Injuries to Mothers
Through my research and interviews with doctors, I learned that birth injuries to mothers can be both physical and psychological. Physical birth injuries include injuries to the perineal area, with first- to fourth-degree perineal tears and episiotomies, which can damage the skin, muscles, and nerves of the perineum. They also encompass injuries to the pelvic floor, such as over-stretching or tearing of pelvic floor muscles, which can lead to pelvic organ prolapse (POP). In some cases, injuries can involve a ruptured uterus or postpartum hemorrhage (PPH). Psychological birth injuries, such as postpartum depression and post-traumatic stress disorder (PTSD), can also result from difficult childbirth experiences. 8 Although I won’t delve into every postpartum injury here, you’ll find a “Further Reading” section at the end of this article with medical sources on this topic.
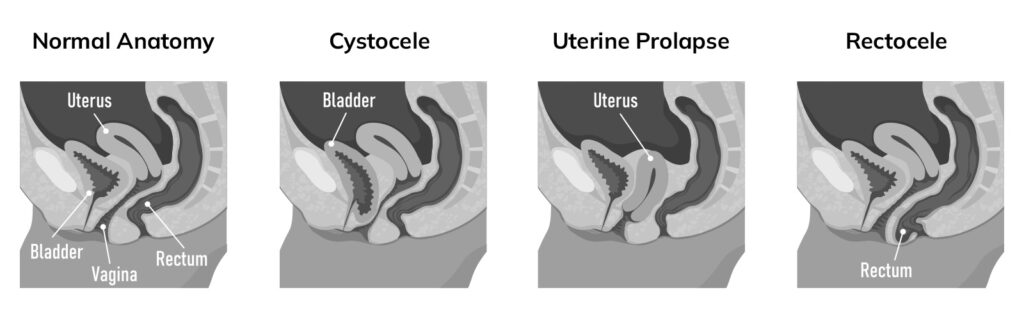
Image source: www.shutterstock.com
Finding help
Every birth injury is unique and requires specific medical attention. It’s crucial to consult a professional, such as a gynecologist or pelvic floor physiotherapist, before trying any treatments mentioned in this article. If your doctor downplays your symptoms or ignores your feelings, find another doctor immediately!
In my case, I dealt with pelvic organ prolapse (POP): cystocele grade II and rectocele grade III. This caused pelvic pain, pressure, painful intercourse, numbness, a foreign body sensation, constipation, and urinary and fecal incontinence. Over 3.5 years, I underwent surgery, physiotherapy, and numerous treatments in Germany, Poland, and Spain, resolving most of my ailments. My recovery is ongoing, and I will update this article with new discoveries. If you have similar problems, consider the following options:
The Pelvic floor physiotherapy
Pelvic floor physiotherapy was the first step in my recovery from childbirth injury, recommended by my gynecologist. I was advised to start strengthening my pelvic floor muscles six weeks after birth. My first physiotherapist was not very helpful; she had limited knowledge about my condition. As with any profession, there are good and bad practitioners, so if you feel you’re not progressing, don’t hesitate to change therapists.
Today, physiotherapists and midwives offer a wide range of services to strengthen pelvic floor muscles, and the internet is full of instructional videos. However, remember that these exercises are not one-size-fits-all. Doing them on your own may cause more harm than good. For example, if the levator ani muscles, which support the pelvic organs, are not intact, pelvic floor exercises may be ineffective or harmful. Effective physiotherapy should include a balanced, individualized exercise plan under the guidance of a healthcare professional.9
Proper pelvic floor physiotherapy should begin with a detailed interview and an examination of the vagina (and sometimes the anus) to ensure you can contract the right muscles. The therapist may also use biofeedback, which involves electronic monitoring devices to provide real-time feedback on muscle functionality and progress. As Luce Brett, the author of the truly remarkable book PMSL: Or How I Literally Pissed Myself Laughing and Survived the Last Taboo to Tell the Tale, says, it’s crucial to be brutally honest with your physiotherapist about your feelings, symptoms, and how you perceive your body. They need to understand your condition fully to help you effectively. 10 Reflecting on my journey, I remember feeling embarrassed and disconnected from my body. Expressing these feelings to my physiotherapist was incredibly challenging, but it was a crucial step towards healing.
Depending on your condition, pelvic floor physiotherapy may include a range of treatments such as:
- Pelvic floor exercises: Developed by Dr. Arnold Kegel in the late 1940s, these exercises involve repeated contraction and relaxation of the pelvic floor muscles.
- Manual therapy: Internal and external massage techniques to release tension and improve muscle function.
- Trigger point therapy: Part of manual therapy, this technique applies pressure to tight knots in muscles to release tension, which was very helpful after my surgery.
- Electrical stimulation: Uses mild electrical currents to reduce muscle spasms and strengthen the pelvic muscles. 11
Early intervention and education about pelvic floor health are crucial for long-term well-being. Learning about your pelvic floor muscles, proper techniques for bladder and bowel management, and activities to avoid that may strain your pelvic floor is fundamental. Don’t rush your recovery; listen to your body and don’t be misled by perfect postpartum bodies on social media. Be kind to yourself—recovering from birth injury takes years, courage, and a lot of patience.

The pelvic floor physiotherapy
Sonja Soeder, German Pelvic Floor Center, Berlin, Germany
Vaginal Pessary
If you are dealing with pelvic organ prolapse (POP) and pelvic floor exercises have had little or no effect on your condition, you may be offered a vaginal pessary. This removable device can support your pelvic organs and prevent further delays in the pelvic floor healing process. Pessary therapy is a non-surgical treatment that immediately reduces symptoms of pelvic organ prolapse and stress incontinence.
There is a wide range of pessaries available in different shapes, forms, and sizes, such as the ring pessary, Gellhorn or Shaatz pessary, Gehrung pessary, donut pessary, and cube pessary. Most are made of silicone. Unlike tampons, most pessaries require an in-office fitting with your gynecologist or physiotherapist. 12 Dr. Lenzen-Schulte points out that despite pessaries being used since the 19th century in forms like wood, rubber, metal, leather, and glass, there are still not many medical practitioners specializing in pessary therapy. 13 Unfortunatelly, this highlights another gap in medical knowledge.
I have never tried a pessary myself, even though it was recommended during my appointment at the German Pelvic Floor Center in Berlin. I was given one to try at home, but as soon as I saw this relatively large and edgy device, I realized it wasn’t an option for me. At that time, I simply couldn’t imagine inserting anything into my vagina. Would it have helped me? Now, I think it could have aided my daily routine and saved me from many embarrassing situations in public, but I wasn’t ready for this type of treatment. However, I know many women of all ages use pessaries with good results, so please make your own informed decision on this matter.
The Magnetic Field Therapy (MFT)
Magnetic Field Therapy (MFT) was a life-changing treatment for me. It was recommended by a Polish gynecologist as my last non-invasive option for treating incontinence and pelvic organ prolapse. The results were revolutionary and significantly improved my life within a few weeks. After just 10 sessions, I was able to stop my urinary and fecal incontinence. I tried both BTL Emsella and PelviPower and can recommend them with similar results.
MFT uses high-intensity focused electromagnetic energy (HIFEM) to stimulate deep pelvic floor muscle contractions, significantly strengthening the entire pelvic floor area and restoring neuromuscular control. Each session lasts about 20-30 minutes, depending on the device or program, and the patient remains fully clothed and seated comfortably throughout. By targeting the deep muscles in the core, this therapy can help improve muscle tone and reduce symptoms of pelvic floor dysfunction. 14 MFT can be expensive and is often not covered by insurance. Many places in Poland, Germany, and Spain offer trial sessions. I recommend trying one first, as you might choose the full package of 10 sessions after experiencing the benefits.
Of course, results and patient experience may vary. While MFT was a breakthrough for me, it had little impact on my mother, who underwent a hysterectomy years ago and sought to improve her urinary incontinence. Unfortunately, in my case, MFT was only a short-term solution. After two years of using this technology, I noticed that pausing my weekly sessions reversed the symptoms of pelvic organ prolapse and incontinence within six weeks. Even though surgery became indispensable for me, MFT was very helpful along the way.
Since MFT is relatively new, we lack long-term data on its effectiveness and potential downsides. Remember that MFT should not replace traditional pelvic floor physiotherapy, which offers a deeper understanding of pelvic floor health and ensures comprehensive care.


Magnetic Field Therapy (MFT) – BTL Emsella
Clinica Serrano, Valencia, Spain
Neural Therapy
Neural therapy is an alternative treatment that uses low-concentration local anesthetics, like procaine, injected into specific areas to treat chronic pain. A few months after birth, I received injections in my vaginal and anal areas to alleviate pain and discomfort from tear or episiotomy scarring, particularly during intercourse. This non-invasive treatment can help women with childbirth-related scars by restoring normal nerve function. 15, 16
In the context of maternal birth injuries, neural therapy is relatively new with mixed results and limited evidence. In Germany, several specialists offer this treatment, but it’s crucial to choose your doctor carefully. Birth injuries often involve emotional trauma, so good injection skills must be paired with a compassionate patient approach. Read reviews and patient feedback before deciding, as my experiences with doctors varied. Despite some negative encounters, neural therapy significantly reduced my pain. Always trust your instincts, and remember you can stop any treatment if it doesn’t feel right.
Neural therapy should complement, not replace, treatments like pelvic floor physiotherapy. Consult your healthcare provider to determine if neural therapy is suitable for you.
Reconstructive Surgery After Birth Injury
In March 2023, I had reconstructive surgery at a private clinic in Warsaw. With a long wait at the German Pelvic Floor Center in Berlin, I opted to go to Poland to end my suffering. Non-surgical treatments hadn’t provided lasting relief for my prolapse symptoms, so I realized surgery was necessary to regain my life. It took months to accept this decision, especially with the risk of surgical scarring, but I was determined to move forward and ease my constant struggle. The surgery involved rebuilding the front vaginal wall with bladder support, fixing the back vaginal wall and perineum with muscle repair, reconstructing the external sphincter, and finally, addressing the clitoral hood. I won’t go into detailed description of the procedure here, but please let me know if you’d like more information in a future article.
Recovery took several months and required frequent visits to the Warsaw clinic. I had to follow a liquid diet for a while to allow the wounds to heal properly. I couldn’t sit on my bottom for the first 6-8 weeks, and walking or bending over caused pain and discomfort. This period was very difficult for me and my family, as I couldn’t lift anything heavy, including carrying my daughter, which saddened both of us.
My reconstructive surgery undoubtedly improved my condition after the birth injury. One year later, bladder and rectal prolapse no longer concerned me. Pelvic pain and urinary incontinence have significantly improved, and my overall quality of life is better. Is this a happy ending? Partly. It feels like laughing through the bad, as I still struggle with some incontinence, pelvic, lower back and hip pain, foreign body feeling and unfortunately, low libido and dyspareunia. Fortunately, I discovered functional and aesthetic gynecology, which is currently helping me improve tissue elasticity in the vagina, enabling a gradual return to intimate life. Finally, I still use Magnetic Field Therapy (MFT) to keep my pelvic floor muscles strong and I will probably continue this therapy until I find a better solution.

Reconstructive Surgery & Doctors performing surgery, Warsaw, Poland
Dr. med. Małgorzata Uchman-Musielak – Specialist in Gynecology
Dr. med. Katarzyna Borycka-Kiciak – Proctology Surgeon
Functional and Aesthetic Gynecology
For women struggling with painful scarring from tears or episiotomies during childbirth, aesthetic gynecology offers a range of vaginal rejuvenation treatments to improve tissue elasticity. Surprisingly, these treatments were never mentioned to me in Germany, but they are more commonly used in Poland and Spain. Regardless of location, your gynecologist can recommend various solutions based on your individual condition. Regenerative, functional, and aesthetic gynecology provides minimally invasive treatments that enhance vaginal and sexual health, self-esteem, and quality of life. Most are painless and require no recovery time, though some need a local anesthetic. These solutions can restore the physical and functional appearance of the vagina, vulva, and pelvic floor:
- Fractional CO2 Laser: Improves natural collagen generation, restoring elasticity and lubrication in the vagina. Reduces scars, dryness, urinary incontinence, and prevents prolapse.
- Fractional Radiofrequency (RF): Painless treatment that can delay aging of female sexual organs and improve urinary incontinence or vaginal dryness.
- Hyaluronic Acid (HA): Enhances tissue regeneration, elasticity, and hydration of vaginal tissues.
- Platelet-Rich Plasma (PRP): Accelerates tissue repair and regeneration, stimulates collagen, and reduces inflammation and pain. Involves injecting concentrated platelets from the patient’s blood into the affected area.
Your doctor may also recommend intimate mesotherapy, involving injections of a mixture of vitamins, enzymes, hormones, and plant extracts, or intimate carboxytherapy, which uses medical-grade carbon dioxide (CO2) injections to improve blood circulation and stimulate collagen production. 17 I have not personally tried these treatments, but they are believed to enhance the health and appearance of intimate areas. Consult your doctor to determine if these treatments are suitable for your specific condition.
Final Words: Where I Am Today?
I have learned so much on this long and bumpy journey. I have faced significant physical and psychological challenges, but the biggest hurdle was dealing with doctors and specialists who dismissed my pain as emotional. Experiencing such misjudgment and ignorance motivated me to co-create No Taboo Mom. This extensive article is the foundation of our platform. I realized that many women suffer in silence, seeking help with little or no support, while others feel misled and uninformed on the journey to motherhood. Sharing my story wasn’t easy, but if it helps even one of you, it was worth it.
Despite some improvements, I continue to face challenges with scarring, pain, and other symptoms while exploring new treatments and therapies. Furthermore, last year, I decided to consult a personal injury attorney to evaluate possible medical negligence during my childbirth. For obvious reasons, I won’t discuss this publicly, but I mention this to highlight that errors can happen, and you have every right to seek legal advice if you suspect a mistake in your case.
My battle is not yet over, but I will keep you updated about my progress and any new treatments that improve my condition. Now, it’s time for you. Have you experienced a maternal birth injury? Or maybe you aren’t sure, but the symptoms sound familiar? Was this article helpful, and did it answer some of your questions? Is there another related subject we should write about? I know this topic is difficult, but if you can, please share your story with us. Your voice matters!
Related articles: Childbirth Stories – From loss of control to total knockout
References :
- Dr. med. Martina Lenzen-Schulte. Untenrum offen – Der Beckenboden nach der Geburt: Verharmlost – ignoriert – tabuisiert. Edel Verlagsgruppe GmbH 2022. p. 18 & p. 49
- https://www.cosmopolitan.com/lifestyle/a61263/how-to-deal-with-childbirth-injuries/
- https://www.ajog.org/article/S0002-9378(22)00464-1/fulltext
- https://www.torbayandsouthdevon.nhs.uk/uploads/23715.pdf
- https://rightasrain.uwmedicine.org/well/health/prolapse-after-pregnancy
- https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(23)00454-0/fulltext
- https://www.pregnancybirthbaby.org.au/birth-injury-to-the-mother
- https://www.mceldrewpurtell.com/news/causes-and-types-of-common-birth-injuries-to-mothers
- Dr. med. Martina Lenzen-Schulte. Untenrum offen – Der Beckenboden nach der Geburt: Verharmlost – ignoriert – tabuisiert. Edel Verlagsgruppe GmbH 2022. p. 59
- Brett, Luce. PMSL: Or How I Literally Pissed Myself Laughing and Survived the Last Taboo to Tell the Tale. Green Tree, Bloomsbury Publishing Plc, UK, 2020, p. 125.
- https://www.webmd.com/women/what-is-pelvic-floor-physical-therapy
- https://my.clevelandclinic.org/health/treatments/16036-pessaries
- Dr. med. Martina Lenzen-Schulte. Untenrum offen – Der Beckenboden nach der Geburt: Verharmlost – ignoriert – tabuisiert. Edel Verlagsgruppe GmbH 2022. p. 57-59
- https://www.maudmedical.com/research-education/the-science-behind-emsella
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7238908/
- https://karger.com/cmr/article/28/6/571/822249/Treatment-of-Localized-Vulvar-Pain-with-Neural
- https://clinicaserrano.com/ginecoestetica-regenerativa/
Further reading :
- MASIC: UK Foundation, supporting women who have suffered serious injuries during childbirth
- Millions of Women Are Injured During Childbirth. Why Aren’t Doctors Diagnosing Them?
- My vagina was badly injured after giving birth. Why was getting help so hard?
- Types of Pelvic Organ Prolapse
- We shouldn’t have to live with ‘broken vaginas’
- Real Talk: Vaginal Tearing during Childbirth
- Birth injury (to the mother)
- Types of Birth Injuries to Mothers
- WHO: More than a third of women experience lasting health problems after childbirth
- Neglected medium-term and long-term consequences of labour and childbirth
- Causes and Types of Common Birth Injuries to Mothers
- The prevention of perineal trauma during vaginal birth
- Birth injuries to mothers: Medical negligence claims
- Surgery for Pelvic Organ Prolapse
- When to see a pelvic floor specialist after birth
- What is Pelvic Floor Physiotherapy and How Does it Work?
- Beckenbodenschäden: Besser als bisher über Risiken vaginaler Geburten aufklären (GERMAN)
Books :
- “Misconceptions: Truth, Lies, and the Unexpected on the Journey to Motherhood” by Naomi Wolf
- PMSL: Or How I Literally Pissed Myself Laughing and Survived the Last Taboo to Tell the Tale by Luce Brett
- “Vagina: A New Biography” by Naomi Wolf
- It’s over – I just don’t know it yet!: coping with traumatic childbirth experiences by Tanja Sahib
- “Untenrum offen: Der Beckenboden nach der Geburt: verharmlost – ignoriert – tabuisiert” (German Edition) by Dr. med. Martina Lenzen-Schulte
Did you like this article?

Meet the Author
Ewa Gillen, co-founder of No Taboo Mom, is a Polish Berliner, creative professional, wife, and mom whose journey into motherhood turned everything around. She holds a Master’s degree in Creative Industries, and having studied, lived, and worked in Poland, Germany, Canada, Australia, and Spain, Ewa brings a rich cultural perspective to her work. As the founder of Gillen Design, she has worked as an Independent Creative Professional for nearly a decade, blending her expertise in design with her passion for meaningful storytelling. “No Taboo Mom is more than a platform—it’s a movement to inspire change through real, open conversations. I believe that by sharing our truths, we create a stronger, more compassionate world for ourselves and the next generation.”